Struggling with itchy, persistent bumps that just won’t go away, no matter what acne treatment you try? It might not be the regular acne you’re used to dealing with—there’s a chance it’s fungal acne.
Surprised?
You’re not alone. Many people mistake fungal acne for traditional acne, only to find out later that the treatments they’ve been using aren’t working because they’re targeting the wrong culprit.
Fungal acne, scientifically known as Malassezia folliculitis, is a skin condition that often flies under the radar. Unlike hormonal or bacterial acne, fungal acne is caused by an overgrowth of yeast on your skin—a fungus that naturally lives on your body but sometimes gets a little out of control.
So why is it important to differentiate fungal acne from the regular kind? Because the treatments are completely different! Understanding what you’re dealing with can save you time, effort, and frustration while helping you achieve clear, healthy skin.
In this blog, we’ll break down everything you need to know about fungal acne: what it is, what causes it, how to identify it, and—most importantly—how to treat it effectively. Ready to get your skin back on track? Let’s dive in!
Have you ever noticed small, stubborn, itchy bumps on your face, chest, or back that just won’t go away, no matter what acne treatment you use? You might be dealing with something called fungal acne or Malassezia folliculitis. While it looks like regular acne, it’s a completely different condition caused by an overgrowth of yeast on your skin.

Fungal acne is a skin condition that occurs when yeast (Malassezia), which naturally lives on your skin, starts growing out of control. Normally, this yeast is harmless and coexists with your skin’s natural flora.
However, when the conditions are right—such as excessive sweating, hot and humid weather, or using antibiotics—it can multiply and cause inflammation in the hair follicles. The result? Small, itchy, red bumps that can look like regular acne but feel much itchier and don’t respond to common acne treatments.
It all starts with clogged hair follicles. Sweat, oil, and dead skin cells create the perfect environment for Malassezia to thrive. Once the yeast begins to overgrow, it irritates the skin and triggers those uniform, red bumps that are characteristic of fungal acne.
It’s easy to confuse fungal acne with hormonal acne, but the two are very different. While hormonal acne is driven by fluctuations in hormones—especially during puberty, menstruation, or stress—fungal acne has nothing to do with hormones. Here’s how they differ:
Fungal Acne | Hormonal Acne |
Caused by yeast (Malassezia) | Caused by hormonal fluctuations |
Small, uniform, itchy bumps | Larger, inflamed pimples or cysts |
Appears on oily areas: chest, back, face | Typically on the jawline, chin, or T-zone |
Worsens with sweat, heat, and humidity | Can flare up with hormonal changes |
Treating fungal acne with the wrong products—like benzoyl peroxide or salicylic acid—can make it worse. Since fungal acne is caused by yeast, it needs antifungal treatments, not typical acne remedies. Misidentifying fungal acne can lead to more frustration and persistent breakouts.
Now that you know what fungal acne is, let’s uncover what causes it to appear in the first place
Have you ever wondered why fungal acne seems to pop up out of nowhere, especially during those hot and humid days? The culprit is a perfect storm of factors that create an ideal environment for yeast overgrowth on your skin. Let’s break it down.
Fungal acne is triggered when the balance of microorganisms on your skin is disrupted. The yeast (Malassezia) that naturally lives on your skin starts multiplying excessively, leading to inflammation in the hair follicles. But what causes this imbalance? Here are the main culprits:
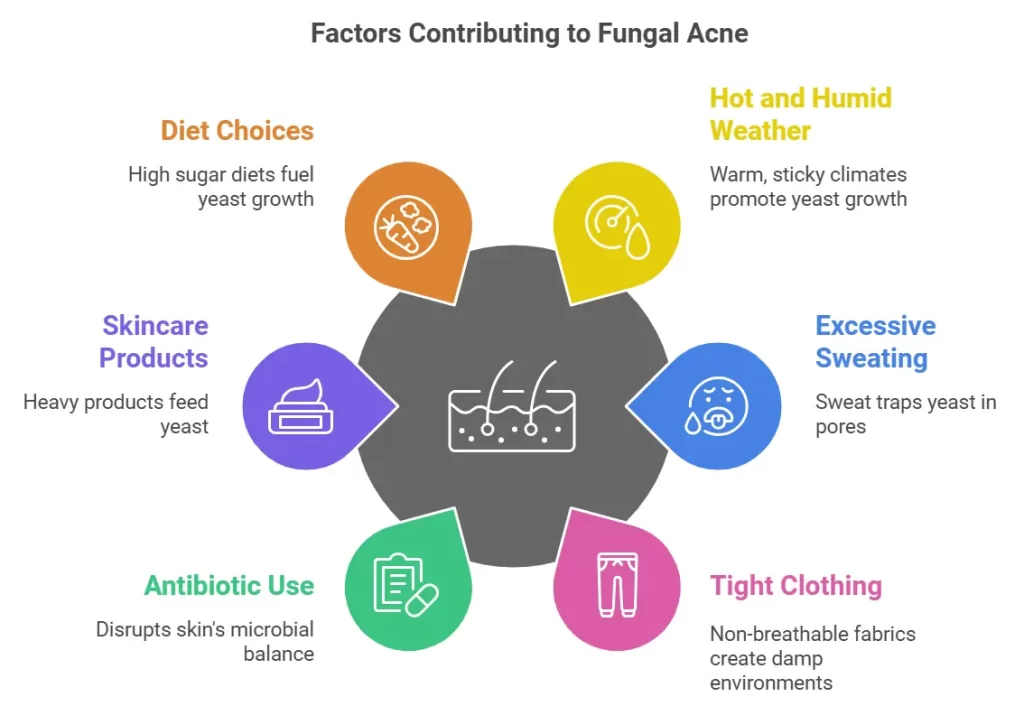
Warm, sticky climates are a paradise for yeast growth. The sweat and oil that build up on your skin create the perfect breeding ground for Malassezia. That’s why fungal acne tends to flare up in tropical or summer conditions.
Do you work out often or sweat a lot during the day? Sweat-soaked clothes and unwashed skin can trap yeast in your pores, causing it to thrive.
Tight clothing or fabrics that don’t let your skin breathe—like polyester or spandex—can trap moisture and heat. This creates a warm, damp environment where yeast can flourish.
While antibiotics are great for fighting bacterial infections, they can disrupt the balance of bacteria and yeast on your skin. Killing off bacteria can give yeast the upper hand, leading to overgrowth.
Heavy or occlusive skincare products, especially those containing oils, can feed the yeast and worsen fungal acne. Products not labeled as “non-comedogenic” or “lightweight” may be problematic.
Believe it or not, what you eat can influence fungal acne. Diets high in sugar or refined carbs can fuel yeast growth, making your breakouts worse. On the flip side, cutting back on sugary snacks might help keep fungal acne in check.
A compromised immune system can make it harder for your body to keep yeast in balance, leading to fungal acne flare-ups.
Stress itself doesn’t directly cause fungal acne, but it can weaken your immune system and make your skin more susceptible to infections, including yeast overgrowth. So, while stress may not be the root cause, it can definitely be a contributing factor.
Diets rich in sugar, dairy, and refined carbs can fuel yeast growth and make fungal acne worse. Think pastries, sugary drinks, white bread, and even certain alcoholic beverages like beer, which contain yeast. Avoiding these foods might help keep fungal acne under control.
Fungal acne isn’t just about what’s happening on your skin—it’s also influenced by your environment, habits, and even diet. By addressing these root causes, you can take the first step toward clearer skin.
Next, we’ll discuss how to identify fungal acne and ensure that you’re not mistaking it for something else!
So, you’re dealing with those pesky bumps on your skin, and you’re wondering—how do I know if it’s fungal acne? Don’t worry; identifying fungal acne doesn’t have to be a guessing game. Here’s a guide to help you spot the difference and determine if what you’re experiencing is indeed fungal acne.
Fungal acne has a few telltale signs that set it apart from other skin conditions. Here’s what to look out for:
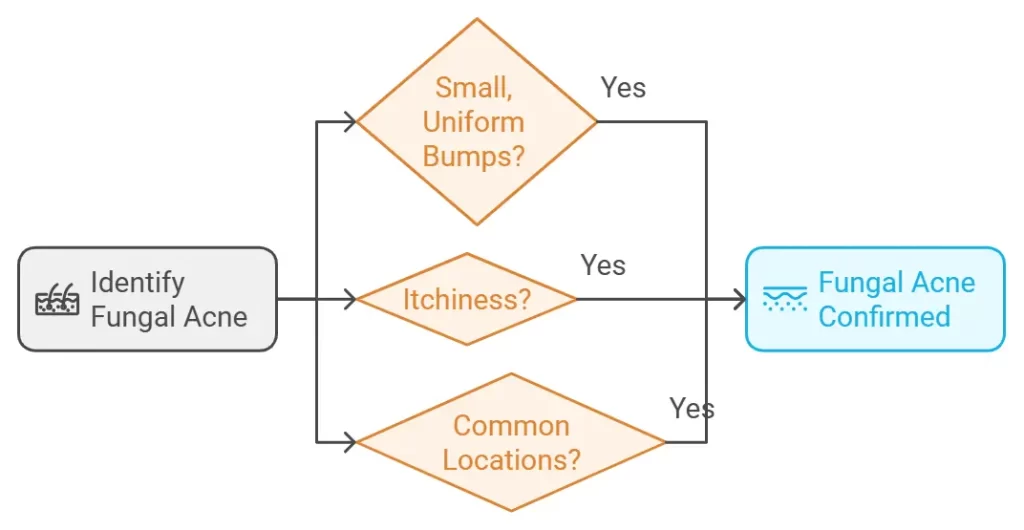
Fungal acne typically appears as small, red, or skin-coloured bumps that are all roughly the same size. Unlike bacterial acne, you won’t find large, inflamed pimples or cysts.
One of the most noticeable symptoms is itchiness. If those bumps are unusually itchy, fungal acne is a strong indicator.
Fungal acne loves areas where sweat and oil accumulate, such as:
Still not sure if it’s fungal acne? Here’s how to tell the difference:
Fungal Acne | Bacterial/Hormonal Acne |
Small, uniform, itchy bumps | Mixed sizes: cysts, whiteheads, or blackheads |
Appears in clusters | Scattered across different areas |
Located on oily, sweaty areas | Often on the jawline or T-zone |
Worsens with antibiotics | Improves with antibiotics |
If your acne flares up after taking antibiotics, it’s likely fungal. Antibiotics can kill off the good bacteria that keep yeast in check, causing it to overgrow.
If you’re still unsure, here’s what you can do:
Try using an over-the-counter antifungal product, like a shampoo containing selenium sulfide or ketoconazole, on the affected area. If the bumps improve within a week or two, it’s likely fungal acne.
For a definitive answer, visit a dermatologist. They can perform a test called a potassium hydroxide (KOH) prep to confirm if yeast is the cause of your acne.
Antifungal creams like clotrimazole or miconazole can help if you’re leaning toward fungal acne. These are readily available over the counter and specifically target yeast infections on the skin.
Understanding these symptoms and knowing where to look, you’ll be better equipped to identify fungal acne and differentiate it from other skin conditions. Up next, let’s explore the different ways to treat fungal acne effectively!
Once you’ve identified that those stubborn, itchy bumps are indeed fungal acne, the next step is tackling it head-on. Thankfully, fungal acne can be treated effectively with the right products, habits, and sometimes professional help. Here’s how to clear it up and prevent it from coming back.
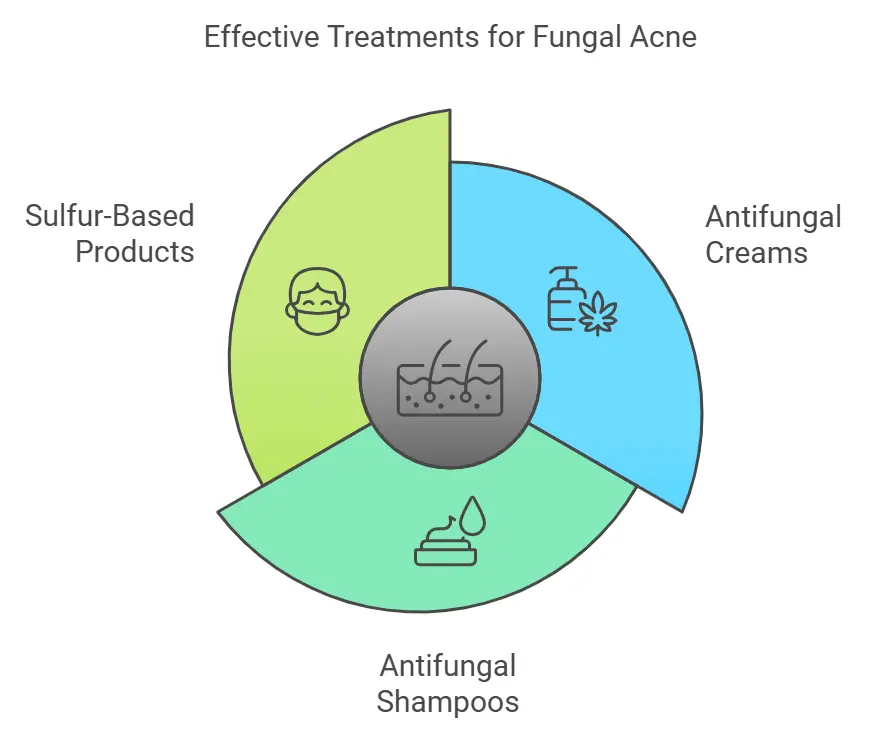
Look for creams containing active ingredients like clotrimazole or miconazole. These ingredients target the yeast that causes fungal acne. For optimal results, apply the creams directly to the affected areas twice a day.
Believe it or not, shampoos like selenium sulfide (Selsun Blue) or ketoconazole (Nizoral) can be game-changers. Use them as body wash on the affected areas, letting the lather sit for 2–3 minutes before rinsing.
Sulfur has antifungal properties and can help reduce inflammation and clear up fungal acne. Look for cleansers or masks with sulfur as the main ingredient.
Prefer natural solutions? Here are some options:
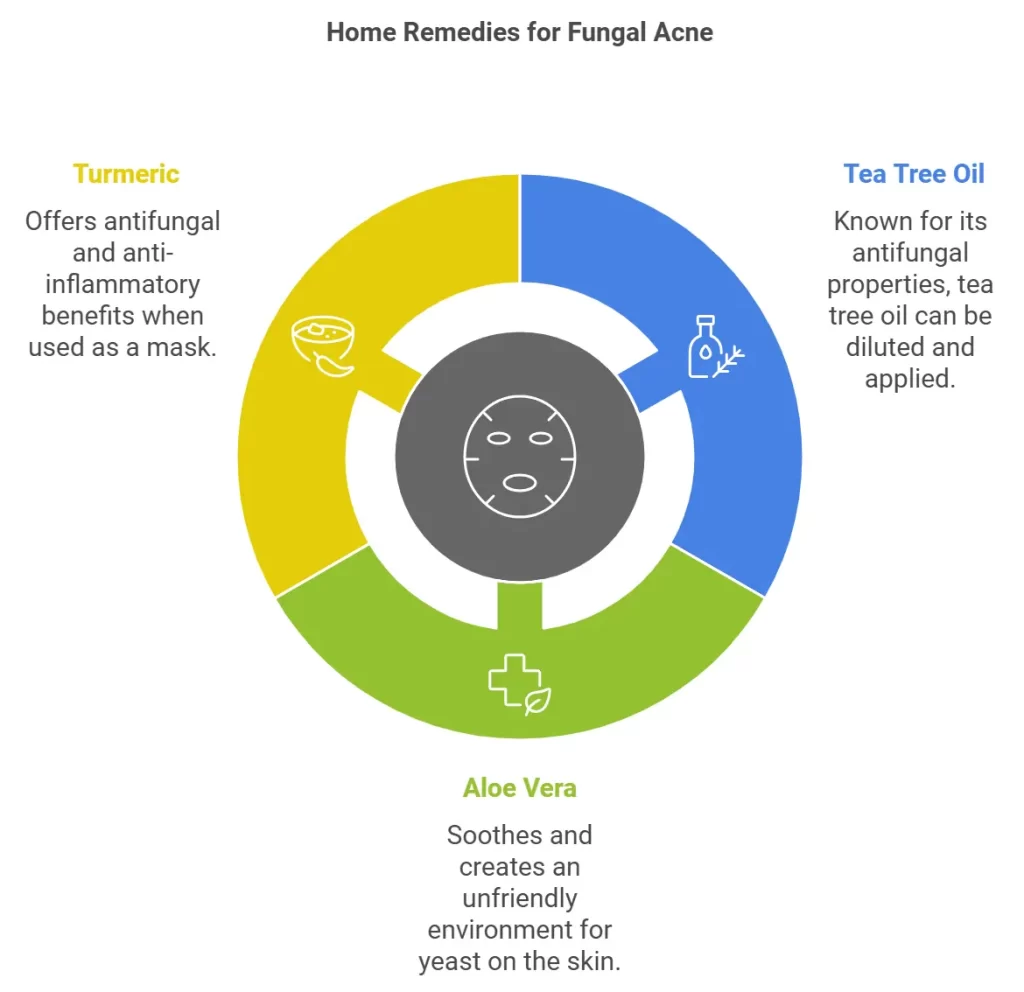
Known for its antifungal properties, tea tree oil can be diluted with a carrier oil (like coconut oil) and applied to the affected area.
Aloe vera’s soothing and anti-inflammatory properties can help relieve the itchiness of fungal acne. While it doesn’t kill yeast, it creates a less hospitable environment for it.
Turmeric has natural antifungal and anti-inflammatory properties. Mix turmeric powder with water or yogurt to create a mask and apply it to the affected area.
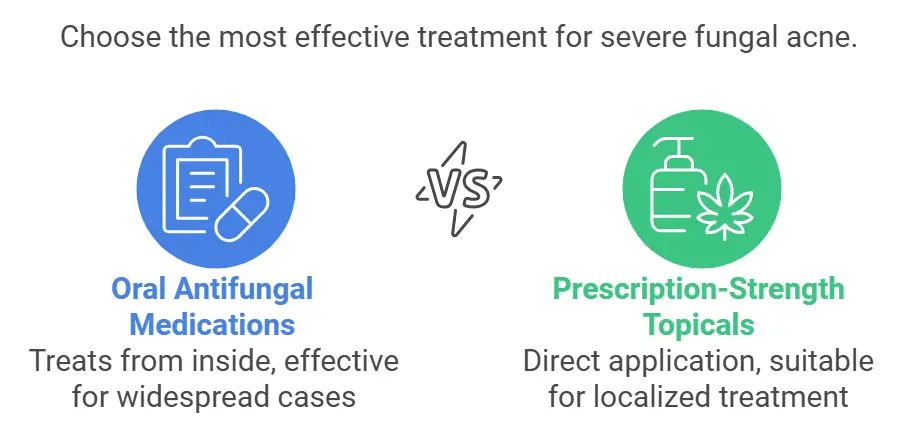
For more severe or persistent fungal acne, a dermatologist may recommend:
Medications like fluconazole or itraconazole can treat fungal acne from the inside out, especially for widespread or stubborn cases.
Your dermatologist might suggest stronger topical antifungals that aren’t available over the counter.
Treatments work best when paired with some key lifestyle tweaks:
Yeast thrives in sweat, so rinse it off as soon as possible after exercising or being in a hot environment.
Choose lightweight, natural fabrics like cotton to prevent trapping moisture against your skin.
Skip heavy oils and greasy creams. Instead, stick to lightweight, non-comedogenic products that won’t feed the yeast.
Combining these treatments with a little patience allows you to control fungal acne and restore your skin to its healthy, clear self. Next, let’s explore how you can prevent fungal acne from returning.
Prevention is always better than cure, especially when it comes to fungal acne. Once you’ve cleared up your skin, keeping fungal acne at bay requires some simple but effective changes to your skincare routine and lifestyle. Let’s dive into the best prevention tips!
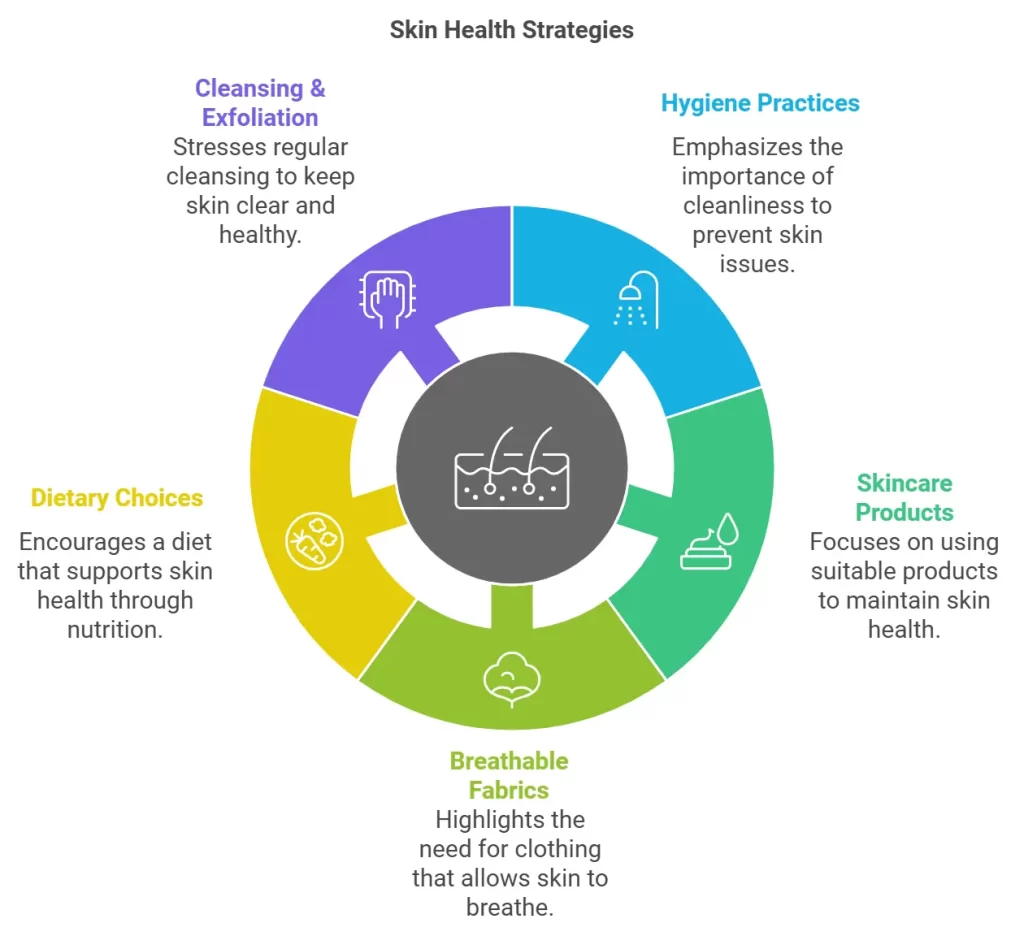
Good hygiene plays a massive role in preventing fungal acne. Here’s how you can stay ahead:
Whether it’s after a workout, a humid day, or heavy sweating, showering immediately helps wash away the sweat and oil that yeast thrives on.
Incorporate products like selenium sulfide or ketoconazole shampoos into your routine once a week to keep yeast in check.
Damp, sweaty fabrics can harbour yeast. Always wear fresh, breathable clothes and wash your towels often.
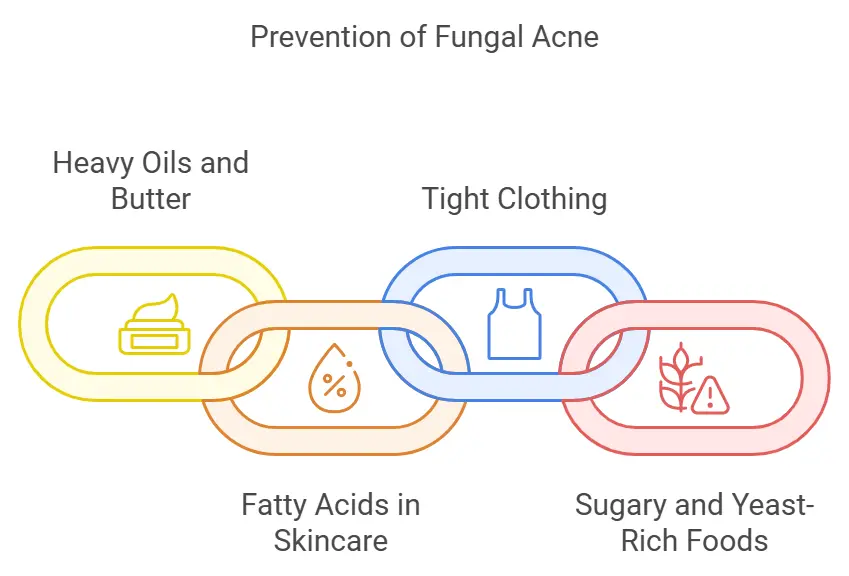
Some skincare habits and products can encourage yeast overgrowth, so it’s important to be mindful of your choices:
Heavy, oily products can feed the yeast. If you’re prone to fungal acne, opt for lightweight moisturizers and avoid occlusive ingredients like coconut oil.
While exfoliation is good for unclogging pores, overdoing it can disrupt your skin’s barrier, making it easier for yeast to overgrow. Stick to gentle exfoliation once or twice a week.
Your clothing matters more than you might think. Tight, synthetic fabrics trap heat and moisture, creating the perfect environment for fungal growth. Choose loose-fitting, breathable fabrics like cotton, especially if you’re in a hot or humid climate.
Believe it or not, what you eat can impact your skin’s balance.
High sugar intake can feed yeast and potentially worsen fungal acne. Minimize sugary snacks, refined carbs, and alcohol.
To support skin health, incorporate foods with probiotics (like yogurt) and those rich in vitamins A, C, and E.
While it’s important not to overdo it, keeping your skin clean and free of excess oil is crucial:
Opt for antifungal or pH-balanced cleansers to maintain the right environment for your skin.
Use a mild exfoliant to remove dead skin cells and sweat buildup that could trap yeast.
Soaps containing sulfur, tea tree oil, or antifungal ingredients like zinc pyrithione are great options.
Avoid high-sugar foods, white bread, and beer, as these can encourage yeast growth.
Scrubbing too hard can irritate your skin and make fungal acne worse. Gentle exfoliation is key.
Preventing fungal acne is all about maintaining balance—on your skin and in your habits. By following these tips, you can significantly reduce the chances of fungal acne coming back.
Next, we’ll debunk some common myths about fungal acne and answer frequently asked questions to clear up any lingering doubts!
Fungal acne is one of those skin conditions that’s often misunderstood, leading to myths and confusion. Let’s bust some of the most common myths and answer frequently asked questions to clear things up once and for all.
This is absolutely not true. With proper treatment and preventative measures, fungal acne can be completely cleared up. However, without addressing the underlying causes, it may recur.
Not at all! Fungal acne isn’t caused by bacteria or clogged pores like traditional acne. Using benzoyl peroxide or salicylic acid can sometimes make it worse because they don’t address the yeast responsible for fungal acne.
Fungal acne can affect anyone, regardless of age. It’s more common in people living in hot, humid climates or those who sweat excessively, but it isn’t restricted to any age group.
While fungal acne is technically not true acne, it presents with similar symptoms (like bumps on the skin). That’s why it’s often referred to as “acne,” even though it’s caused by yeast.
Fungal acne rarely goes away without intervention. Since it’s caused by yeast overgrowth, the right antifungal treatment is necessary to eliminate it.
Start with simple steps like:
The fastest way to address fungal acne is by using products with antifungal ingredients like ketoconazole, selenium sulfide, or zinc pyrithione. Consistency is key—apply these treatments regularly for noticeable results.
Yes, fungal acne is a fairly common condition. It’s just often overlooked or misdiagnosed because it looks so similar to traditional acne.
Stress itself doesn’t directly cause fungal acne, but it can weaken your immune system, making it easier for yeast to grow unchecked.
Yes! Unlike traditional acne, fungal acne is often intensely itchy, which is one of its distinguishing characteristics.
There is a lot of misinformation about fungal acne, but understanding the facts can make a world of difference in treating and preventing it. If you’re still struggling despite trying these solutions, consulting a dermatologist can provide clarity and customised care.
Up next, we’ll discuss the perfect skincare routine tailored specifically for fungal acne!
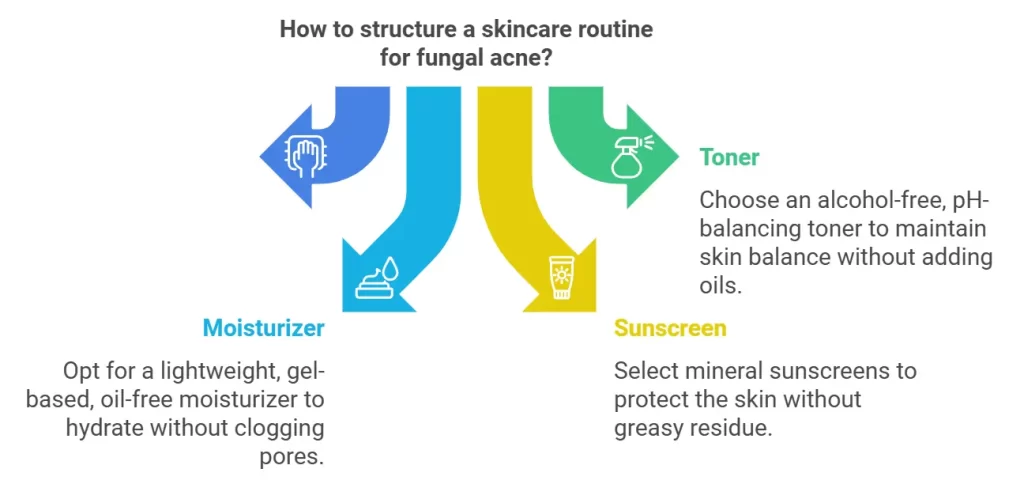
Getting fungal acne under control requires not just treatment but a thoughtful, consistent skincare routine. The right products and steps can help reduce yeast overgrowth, soothe your skin, and prevent future flare-ups. Let’s dive into a skincare routine tailored for fungal acne.
Use a gentle, antifungal cleanser to start your day. Look for ingredients like:
If you prefer a toner, go for an alcohol-free, pH-balancing formula to reduce irritation. Avoid toners with oils or heavy fragrances, which can aggravate fungal acne
Choose a non-comedogenic, oil-free moisturizer. Gel-based moisturizers with ingredients like hyaluronic acid work well without clogging pores or feeding yeast.
Protect your skin with a broad-spectrum sunscreen. Opt for mineral sunscreens containing zinc oxide or titanium dioxide—they’re gentle and don’t encourage yeast growth. Avoid greasy or heavy sunscreens.
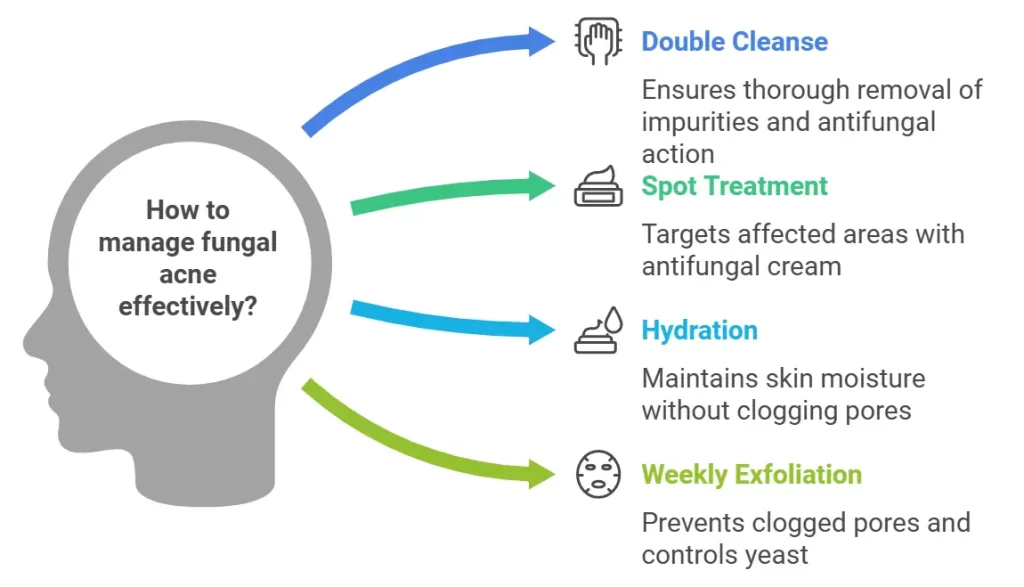
Apply an antifungal cream (like clotrimazole) to affected areas. If your dermatologist prescribed a stronger antifungal, follow their instructions.
Even at night, fungal acne-prone skin benefits from lightweight, non-oily hydration. Look for water-based moisturizers or serums.
Exfoliate gently 1–2 times a week to prevent clogged pores. Use a product with:
Some skincare products can exacerbate fungal acne. Steer clear of:
Cleansers containing ketoconazole, sulfur, or zinc pyrithione are the best options for keeping fungal acne under control.
Yes, but choose lightweight, non-comedogenic products labeled “oil-free.” Always remove makeup thoroughly at the end of the day.
Absolutely! Even oily skin needs hydration. Opt for gel-based, water-light moisturizers that don’t clog pores or feed yeast.
Retinol can help improve skin texture, but it doesn’t directly treat fungal acne. Use it cautiously and avoid combining it with antifungal creams unless advised by a dermatologist.
Stress itself doesn’t directly cause fungal acne, but it can weaken your immune system, making it easier for yeast to grow unchecked.
Yes! Unlike traditional acne, fungal acne is often intensely itchy, which is one of its distinguishing characteristics.
A fungal-acne-friendly skincare routine is all about balance: keeping your skin clean, hydrated, and free from ingredients that feed yeast. With a consistent routine and the right products, you’ll treat fungal acne and keep it from coming back.
Next, let’s address some other common concerns and questions about fungal acne, like whether ice, steam, or diet can help manage it!
Fungal acne often raises many “what ifs” and “can I?” questions. From home remedies to diet and skincare habits, let’s clarify some common concerns and help you make informed decisions about managing fungal acne.
Yes, aloe vera has mild antifungal properties, but its primary benefit lies in soothing irritated skin. While it won’t directly eliminate fungal acne, it can help reduce inflammation and itchiness, making your skin feel more comfortable. Apply pure aloe vera gel to the affected area for a cooling effect.
Ice won’t kill the yeast causing fungal acne, but it can temporarily reduce inflammation and soothe itchiness. Wrap ice in a clean cloth and apply it gently to the affected area for a few minutes. However, ice is a short-term solution and won’t replace proper antifungal treatments.
To keep fungal acne from worsening, avoid:
Steam can actually make fungal acne worse. The warm, moist environment created by steam can encourage yeast growth. Instead of steaming, focus on gentle cleansing and keeping your skin dry.
Yes, diet can play a role in fungal acne management. High-sugar and high-carb diets can fuel yeast growth, making fungal acne more difficult to control. Try incorporating more:
When choosing skincare products, look for these fungal-safe ingredients:
Home remedies can complement medical treatments but aren’t standalone solutions. For example:
Always patch-test before trying a new remedy to avoid irritation.
Fungal acne isn’t just about what you put on your skin—your habits, environment, and diet also influence it. Avoiding triggers like occlusive products, excessive heat, and sugary foods can make a significant difference. Combine these preventative steps with a proper skincare routine to keep fungal acne under control.
Next, we’ll discuss when it’s time to see a dermatologist and how they can help diagnose and treat fungal acne effectively!
While over-the-counter treatments and lifestyle changes can often help manage fungal acne, there are times when professional guidance is necessary. Persistent or severe cases of fungal acne may require a dermatologist’s expertise to get your skin back on track. Here’s how to know when it’s time to seek help.

If you’ve been using antifungal treatments for several weeks and see little to no improvement, a dermatologist can help identify whether it’s truly fungal acne or another condition with similar symptoms.
When fungal acne covers large areas of skin—such as the back, chest, and shoulders—or causes significant discomfort, it’s best to consult a professional.
If fungal acne keeps coming back despite treatment, there may be an underlying issue, like an undiagnosed immune system imbalance or lifestyle factor, that needs to be addressed.
Fungal acne can easily be confused with bacterial or hormonal acne. A dermatologist can perform tests to confirm the diagnosis and recommend the appropriate treatment.
Dermatologists have specific tools and techniques to diagnose fungal acne accurately:
A dermatologist may prescribe oral antifungal medications like fluconazole or itraconazole for severe cases. These medications work within the body to tackle yeast overgrowth.
Prescription-strength antifungal creams, such as econazole or ciclopirox, may be recommended for persistent fungal acne.
A dermatologist can create a skincare routine tailored to your skin type, environment, and triggers, ensuring long-term control of fungal acne.
Sometimes, fungal acne is linked to conditions like weakened immunity, excessive sweating, or lifestyle habits. A dermatologist can help identify and address these root causes.
If your acne doesn’t respond to antifungal treatments within 2–3 weeks, or if it’s causing significant discomfort, it’s time to consult a professional.
Yes, because it looks very similar to bacterial or hormonal acne. A dermatologist’s expertise and diagnostic tools can ensure you’re treating the right condition.
Not necessarily. Many cases of fungal acne clear up within weeks of proper treatment. However, your dermatologist may recommend ongoing preventative steps, like using antifungal shampoos or avoiding certain skincare products.
Don’t hesitate to see a dermatologist if your fungal acne persists or worsens. Accurate diagnosis and targeted treatments can help you achieve clear, healthy skin—and guide you in preventing future flare-ups.
Fungal acne might seem like a frustrating mystery at first, but understanding what it is and how it works makes all the difference. Unlike traditional acne, fungal acne is caused by yeast overgrowth, and treating it requires a completely different approach.
From identifying the small, itchy, uniform bumps to understanding the root causes—like humid weather, sweat, and even diet—you now have the knowledge to take control of your skin. Remember, the right treatments, such as antifungal creams or shampoos, paired with lifestyle changes like breathable clothing and proper hygiene, can clear up fungal acne effectively.
If you’re still struggling or unsure about your condition, don’t hesitate to consult a dermatologist. They can help diagnose your skin concerns and provide tailored solutions for lasting results.
Book An Appointment